For Dr Jogin Desai, CEO and co-founder of Eyestem, a leading Indian cell therapy company, a meeting in 2015 with ophthalmologist Dr Rajani Battu for a medical appointment changed everything. Following the appointment, she introduced him to patients diagnosed with degenerative diseases of the eye and the terrible suffering they have to endure.
It was an eye-opener for Desai, a native of Ahmedabad and an expert in the field of drug development. Desai, at the time, was CEO of Cenduit, an industry leader in the IRT (interactive response technology) market and the eClinical field.
“From school students who cannot see their blackboards to families with children suffering from blindness because of genetic disorders and senior citizens who have lost all agency due to their inability to read, the conversation opened my eyes to a world that I didn’t know existed. In the same week, I met Prof S. Ramaswamy at Instem (Institute for Stem Cell and Regenerative Medicine), again for something completely unrelated, and we discussed the possibilities of how the next two-three decades will evolve with the maturation of cell and gene therapy products worldwide,” recalls Desai, in a conversation with The Better India.
Following the meeting, it dawned on Desai at the time that the world is on the cusp of a fundamental change in the healthcare landscape that will evolve over the next few decades.
Today, Dr Rajani Battu is the chief medical officer at Eyestem.
“Diseases that were previously incurable will start becoming curable. As I dove deeper, I understood that most of these therapies developed in the West will cost upwards of $450,000 (about Rs 3.5 Crore) per injection. This, I believe, presented a once-in-a-lifetime opportunity for a platform that can help disrupt this paradigm and create an incredible impact on the lives of patients. I made the decision to establish Eyestem within two days of these meetings in late 2015,” adds Desai.
Eyestem’s vision is to create a scalable cell therapy platform to treat incurable diseases and democratise access to these newer technologies.
Incorporated in late 2015, Eyestem started operations in early 2017.
“As cell and gene therapies become available across the world, they will only be available to the top 0.01 % of the world’s population. Our purpose is simple: We aim to democratise access by creating a therapy that is available to a large part of the bottom 99.99% of the population in the world. To our knowledge, we are the only company in the world with such a mission. While it is hard to predict the price of the therapy at this stage we anticipate the therapy to cost 80-90% cheaper than such comparable therapies in the West. The only purpose to start Eyestem has been ensuring that the therapy reaches the people that need it the most,” claims Desai.
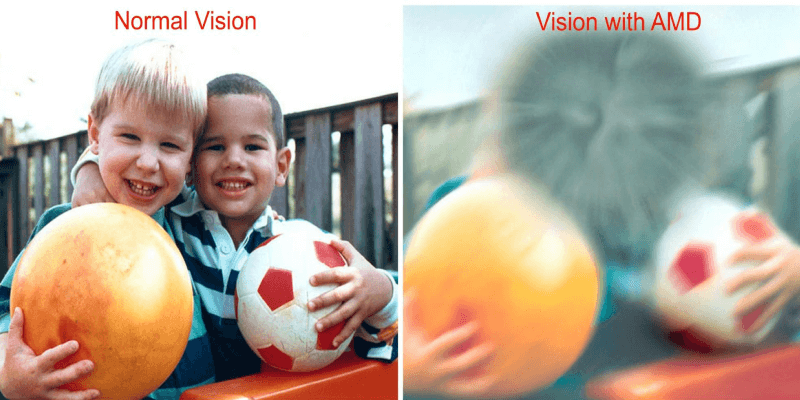
Through its flagship product Eyecyte-RPE, the company replaces lost retinal pigment epithelium cells. It is designed to restore sight for patients in the early stages of Age-Related Macular Degeneration (AMD) and arrest losses for those in the later stages.
“There is no cure for Dry Age-Related Macular Degeneration in the world. It is the largest cause of blindness for people over 50. It is estimated that over 170 million people (40 million of which are in India) suffer from this disease. Eyestem is looking to take Eyecyte-RPE for Dry AMD through clinical trials and is one of six companies worldwide pursuing this treatment,” he says.
Underpinning this type of treatment are Induced-Pluripotent Stem Cell (iPSC)-based products. An iPSC is a cell that can be developed into any cell of the body. At present, there are no iPSC-based products approved anywhere in the world.
Over the next ten years, Desai explains that several such products will start becoming available in the market and diseases such as inherited blindness/pulmonary fibrosis/diabetes which were hitherto considered incurable will start becoming curable.
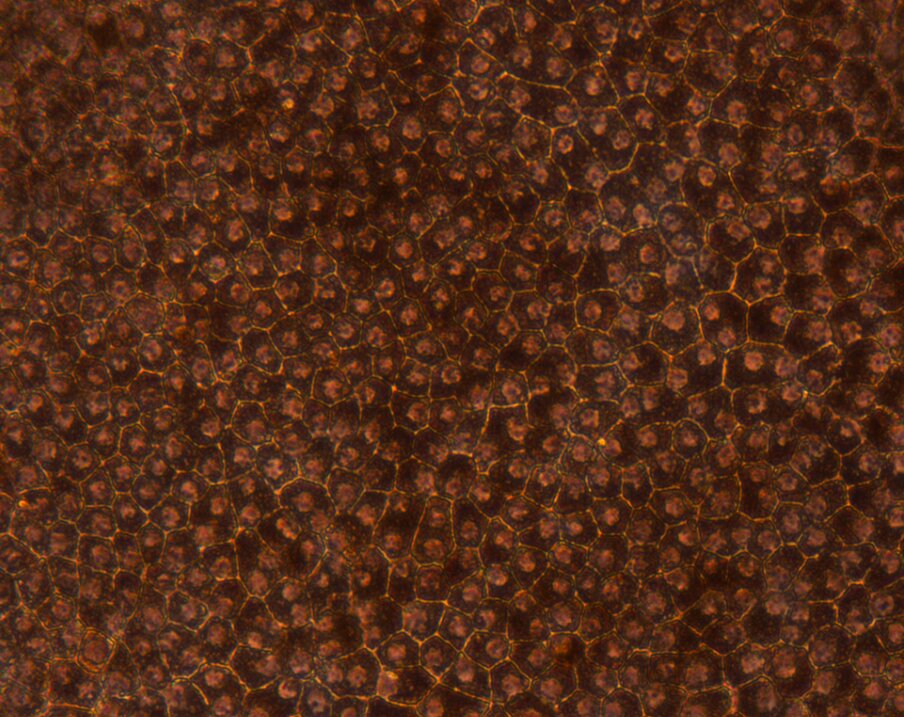
“Subsequently, an explosion in iPSC based therapeutics combined with gene engineering will be the next wave of pharma innovation. A lot of diseases occur when the cells of our body die early or are malfunctioning. At its most basic detail, one can create tissue of any kind (be it brain, heart, lung, eye, liver, kidney) through iPSC and replace the lost/damaged cells of the body. For example, in Dry AMD, the RPE layer degenerates and our treatment would be to inject that layer (from a healthy donor) back into the body part to treat the disease,” he explains.

Curing Incurable Blindness and Other Diseases
So, how does Eyestem’s flagship product, Eyecte-RPE, work as a mode of treatment?
The Retinal Pigment Epithelium (RPE) is one of ten layers of the retina and acts as a foundation on which the rest of the retina sits. In Dry AMD, the RPE layer disintegrates and the retinal layers disintegrate just as a building collapses when the foundation collapses.
“We have grown the RPE layer in our lab and this is Eyecyte-RPE, our flagship product. This product has been injected into special models of blind rats. We have proven that the rats where our product is injected can retain their sight while the ones that are controlled rats go blind. This animal experiment has been done at Oregon Health and Science University which is a global centre of excellence for macular degeneration research. The DCGI (Drugs Controller General of India) has approved manufacturing only for clinical trials and we have not yet applied for commercial manufacturing,” he explains.
In addition to this, Eyestem is also among one of five companies globally advancing the treatment of Retinitis Pigmentosa (RP) to the market called Eyecyte-PRP. Eyecyte-PRP replaces the photoreceptor cells that are lost as a consequence of this disease. RP is a group of rare, genetic disorders that involve loss of the light-sensing photoreceptor cells in the retina. It affects children and causes total blindness by the time they reach their 20s and 30s. It is estimated to affect 4 million children worldwide, of which 1.5 million are in India. Human trials for Eyecyte-PRP to treat retinitis pigmentosa is expected to begin in the second half of FY 2023.
Similarly, Eyestem is also looking to treat Idiopathic Pulmonary Fibrosis (IPF), a serious chronic disease that affects the tissue surrounding the alveoli (tiny air sacs in your lungs), with a pluripotent stem cell-based approach.
“Our first human trials for our Aircyte-AEC treatment to treat idiopathic pulmonary fibrosis will begin in the second half of FY2024. Aircyte-AEC is a suspension of lung alveolar epithelial cells that are lost due to this disease. It is worth noting that pulmonary fibrosis occurs as an end-stage event in several other diseases like COVID-19, Tuberculosis and Chronic Obstructive Pulmonary Disease,” notes Desai.
Meanwhile, for the sake of clarification, we asked Desai whether cell therapy necessarily means stem cell therapy? “Yes, it means the same from a layman’s perspective. The only difference is that there are clinics that advertise ‘stem cell therapy’ for patients in India as well as the US. It is important to remember that none of these stem cell therapy products are approved by the DCGI in India or the FDA in the United States,” he notes.
State of Cell Therapy in India, Funding and Moving Ahead
There are only a handful of companies in India that are pursuing cell therapy. According to Desai, the developed world, especially countries like Israel, Japan and the United States, are at least two decades ahead of India in that regard.
“As more incurable diseases become curable (think diabetes or cancer) it is absolutely imperative for India to develop a base of such product development research or else we will find ourselves in a situation similar to the HIV epidemic (and cell therapy is not easy to reverse engineer unlike HIV medicines). Our patients will be at the mercy of predatory pricing of global pharma unless globally innovative products are manufactured and made available locally. Our nine-member team at Eyestem, a majority of whom are cell biology scientists specializing in this field, is looking to significantly address this issue in advance,” says Desai.
Meanwhile, Desai claims that his venture has been very selective in raising funds so far since its purpose is not to raise “rounds of money with higher valuations but to benefit end patients”. They are ‘laser-focused’ on creating affordable cell therapy and hence have set themselves a benchmark of not spending more than $4 million from idea to first in human trials. Most pharmaceutical companies, he claims, spend 10 times this amount to reach this stage.

“Any drug development venture needs smart money. We were fortunate to have interest from a group of investors who have multi-decade experience in global drug development. Two institutional investors (Endiya Partners and Kotak Private Equity) joined in a subsequent pre-series A round. We are currently raising our series A and we are halfway there. About 30% has been committed by current shareholders and we have a soft commitment from a global venture fund for the other 20%. We anticipate closing this round in the next 8-12 weeks. Investors invest in ventures like ours due to the promise of immense market potential for these therapies. As soon as one obtains human data, startups like ourselves reach an inflexion point and become extremely valuable,” claims Desai.
Please Note: The Better India does not verify for the future efficacy of any therapy or medical treatment mentioned in the article. Kindly consult your doctor for an informed medical opinion.
(Edited by Vinayak Hegde)
No comments:
Post a Comment