This article is sponsored by Bayer
India’s rural healthcare system is strained due to a severe shortage of doctors and infrastructure. The Government’s Rural Health Statistics 2021-2022 report reveals a deficit of 79.5 percent in rural healthcare specialists.
Primary Health Centres (PHC), the initial point of care for villages, cater to around 36,000 people per PHC, as per the same report. PHCs typically have one medical officer who is a physician, staff nurses, and Auxiliary Nurses and Midwives (ANM) along with other staff members.
Inadequate infrastructure and a high patient load contribute to significant stress on doctors and nurses. Villagers have to travel for about 45 minutes to reach the nearest district hospital to access a specialist. To address these issues, Bayer Foundation India (BFI) has established telemedicine centres at PHCs to bring top healthcare professionals to local communities, right at their doorstep.
Sarita Bahl — Country Group CSR Head, Bayer, South Asia & Director, Bayer Foundation India — says, “We travelled to many districts across the country like Raichur, Khandwa, and Tikamgarh, and saw that there was very little support available in PHCs. People have to travel several kilometres just to see a specialist, and many may not go. So we realised that rather than building something new, we should make healthcare better, affordable and accessible right at the PHC.”
So far, Bayer has set up 28 ‘Phygital’ telemedicine centres in 14 aspirational districts (a programme by the government to improve underdeveloped districts nationwide) across eight states, Sarita tells The Better India.
Strengthening the health index of the rural community

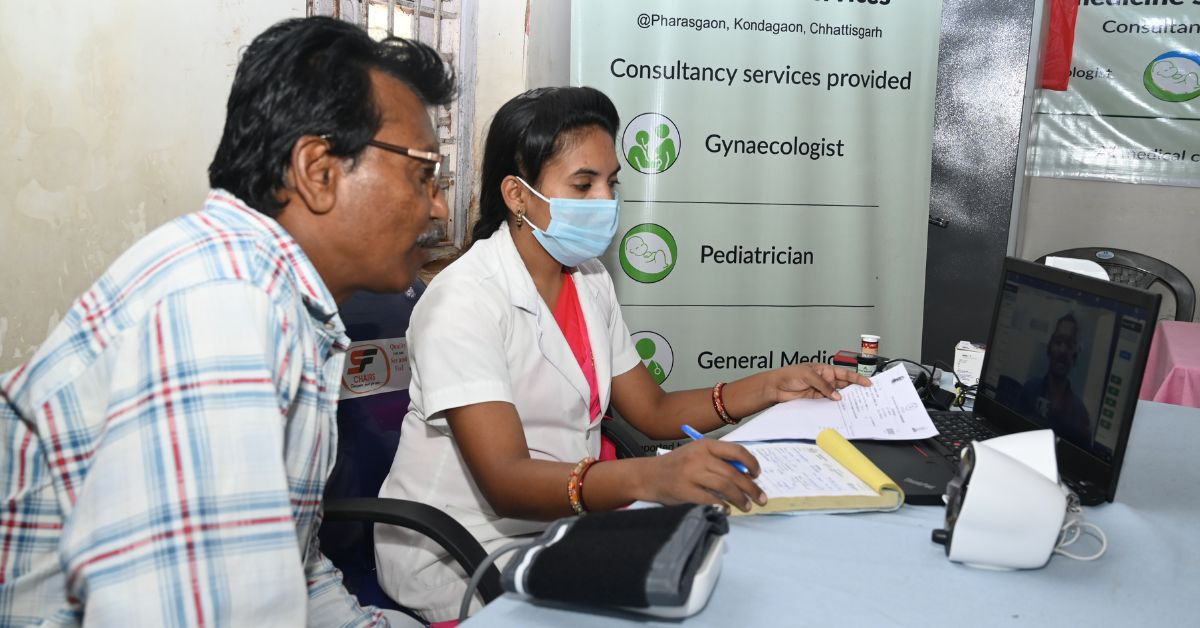
Bayer’s telemedicine centres set up within the PHCs, offer around 20 distinct medical specialities via teleconsultation. The centres include a trained GNM (General Nursing and Midwifery) and a centre coordinator.
As Sarita explains, when a patient requires a specialist’s opinion, they are directed to the telemedicine centre, often located in the adjacent room within the PHC. Here, the nurse links the patients to the specialist via a video call after examining their vital signs and medical background. Post the consultation, the nurse issues a printed prescription to the patient, who can purchase the prescribed medications from the PHC pharmacy.
Falguni, the ANM at the Phygital in Chhiri, Gujarat, emphasises the significant benefits that Bayer’s intervention has brought to the local community and nearby villages. She highlights that patients from remote villages no longer have to endure the trouble of travelling and spending an entire day at the district hospital. With the convenience of accessing various specialists through telemedicine centres, patients have readily embraced this solution. She notes that their PHC witnesses over 90 teleconsultation cases on a daily basis.
Dr Hanifa Batterywala, a ‘Phygital’ doctor, says, “Telemedicine helps us reach even remote areas where often patients are daily wage workers who can’t afford to lose an entire day to travel to see a doctor.”
“After suffering from chronic itching for two months, I spoke to the ANM, Falguni, and she booked a video consultation with a dermatologist. The doctor prescribed a lotion and a medicine. My itching reduced in just three to four days, and I have faced no problem after that,” says Sonal Patel, a patient from Chirri. Falguni adds that most patients seek help for skin allergies or paediatric issues.
Despite the limited timings of the PHCs, Bayer’s ‘Phygital’ centres operate from nine to five, providing access to physicians, gynaecologists, cardiologists, ENT specialists, dermatologists, paediatricians, and other experts via teleconsultation.
Diagnosing silent killers

Bayer’s analysis of data collected from all the PHCs suggested that the highest number of cases at the centres constituted non-communicable diseases (NCDs) such as hypertension and diabetes.
In India, the prevalence of diabetes and hypertension is rapidly increasing, as indicated by a recent ICMR-INDIAB study, which estimates the numbers to be 101 million and 136 million, respectively. The study also highlights that more than one-third of Indians are affected by hypertension, with a high prevalence of prediabetes observed in rural areas.
Diabetes and associated NCDs can lead to cardiovascular complications and other health issues such as kidney, foot, and eye diseases. The report emphasises the critical importance of early diagnosis, prevention and treatment to reduce fatalities caused by these complications.
Working on these tenets is a major part of Bayer’s initiative today. They organise monthly health camps to raise awareness about diabetes, hypertension, various heart conditions, breast cancer, and more.
Sarita informs that since April 2022, they have organised over 539 health camps, reached 6,000 villages, and assisted over 1,70,000 beneficiaries in Bihar, Chhattisgarh, Jharkhand, Karnataka, Gujarat, Uttar Pradesh, Maharashtra, and Madhya Pradesh. These camps involved over 95,000 general consultations and 74,000 specialist consultations. “We want to make sure that no disease goes undiagnosed because of lack of resources or awareness. Quality health care should be available to every person across the country,” says Sarita.
Edited by Pranita Bhat
No comments:
Post a Comment