Trigger warning: The story contains mentions of distressing scenes
“It wasn’t the first time I was watching a baby being delivered. But this delivery was definitely the first of its nature. The mother’s cervix was stitched with a needle and thread — the kind one would use for sewing clothes. Soon after, the woman, who I assumed to be a doctor, nurse, or paramedic, picked up the broom lying on the floor and resumed her duty. I was quick to deduce, the hospital sweeper had just performed the delivery.”
Reliving her first day at the Motihari District Hospital in Bihar gives Dr Taru Jindal the chills. Despite being briefed on the incongruities in the state’s healthcare — Bihar was once infamous for its high infant mortality rates; 42 deaths per 1,000 live births before 2020 — the young gynaecologist hadn’t expected the atrocities on the ground to outdo the theoretics to this degree.
Was she having second thoughts about leaving her cushy life in Mumbai in 2014 in exchange for a project in the hinterlands? “Absolutely,” she reminisces. When she applied for the programme — sponsored by the Bill and Melinda Gates Foundation and managed on the ground by two NGOs, ‘Care-India’ and ‘Doctors For You’ — the mandate was clear: use your medical prowess to train doctors in maternal care.
But, what Dr Taru hadn’t accounted for was the road to this goal being paved with apathy, callousness, and inefficiency. Her initial months in the Motihari District Hospital textured her understanding of the state’s threadbare healthcare systems.
‘Every norm of hygiene was flouted’
How long is 14 days? For Dr Taru, it seemed to span an eternity. With every passing day, she became more and more repulsed. “I would walk into operation theatres where assistants in banyans (vests) were performing surgery. While the patient lay with the abdomen cut open, the room was crowded with ten to twelve people, the patient’s relatives, watching the surgery.”

The very anatomy of the medical policy framework needed a restructuring. But the number of squalid practices made it tough to decide where to begin. People openly urinated in the Labour Room — “When I’d walk in on them, they would continue unperturbed,” faeces lay around the premises and biomedical waste was dumped outside windows.
Dr Taru recounts being “numbed by this sensory overload”. At every corner she was met with heaps of blood-stained clothes, used syringes with needles dangerously jutting out of them, and placental tissue that lay forgotten.
She shudders remembering the day she stumbled upon a post-mortem table that doubled up as an operation theatre table. “Major abdominal surgeries were sometimes performed in dusty rooms which opened into garbage areas that doubled up as toilets and syringes were washed in water; sterilisation was a foreign concept.”

Basic protocol adherence seemed like a fevered delusion. The doctor deduced that years of lackadaisical attitudes had decimated mindsets, culminating in this defunct health infrastructure. One day, she decided to scan the Labour Room and was aghast to discover that it held two artery forceps, one pair of scissors, and one needle holder along with four rusted cots. How this sufficed for the forty-odd deliveries that happened here every single day was beyond her.
“This was supposed to be the largest hospital of the district where mothers from far-flung villages were to be brought for ‘safe delivery’,” she underscores the irony.
At the end of the fortnight, Dr Taru wanted nothing more than to escape the crisis unfolding before her. But an inner voice told her otherwise. This place needed her.
“I realigned my mind. I decided I was not going to sit around and watch this. Instead of worrying whether the system would ever change, I had made up my mind to do something, anything…even if I could just make the hospital cleaner, I would do that,” she shares.

She never booked that return ticket back home. Instead, she stayed on for two years in Bihar, dividing her time between the Motihari District Hospital where she spent six months attempting to reform the policies, and a health centre that she started and ran for a year in the village of Masarhi in Patna. Here, she provided quality medical services to the most impoverished Musahar community.
She never wanted to leave. And she never would have if it weren’t for being diagnosed with a brain tumour. The next few years were filled with extensive rounds of chemotherapy.
Sparking a revolution in Bihar’s healthcare
In 2017, Dr Taru returned to Motihari to collect the luggage she hadn’t been able to take when she left. As she stood at the hospital gates, a sense of déjà vu crept in. She remembered with pride her wide-eyed younger version that had stood in the same spot in 2014, anxious to attempt to change the status quo.

As the staff showed her around the campus, she was impressed. The corridors were sparkling clean; sign boards and health messages offered hope and advice from every corner. “At the entrance of the Labour Room where people once urinated stood a very well-organised nursing station,” she describes. The revolution she had sparked in 2014, had finally had its full-circle moment, it seemed.

The doctor explains that none of this would be possible without systemic changes in the very framework of Bihar’s healthcare. While attempting to wedge out the inequalities and misconduct, her overarching goal was to democratise access to healthcare.
Here’s how Dr Taru bridged the long-standing disparity in the public health policy at Motihari District Hospital, a model that can be replicated in other hinterlands of India.

An attitude change works wonders
Dr Taru is one of the calmest, most composed people I have had the pleasure of interacting with. But, she modestly points out, her emotions weren’t always in check. “I would often get outraged at people who I thought were perpetrators of injustice.” However, her interactions with the locals at the hospital and beyond taught her that constructive action needed patience. “I learnt to rein in my emotions. I realised that before making strategies for external changes, my internal world needed some changes too.”
Create an enabling environment
The two years saw Dr Taru helm multiple training sessions — these focused on sterilisation, measuring blood pressure, checking the baby’s heart rate, reviving the baby, managing the mother’s bleeding after delivery, the basics of hand washing, wearing gloves, making cotton pads, sterilisation of instruments, using the Ambu bag to revive newborns, and managing post-delivery bleeding.
In fact, she later learnt, that the “life-saving” techniques of bimanual compression (technique of squeezing the uterus between one’s hands in vivo) and that of compressing the aorta, became popular methods deployed by the staff to save bleeding mothers.

Traditional mindsets need innovative approaches
Every morning the villagers of Masarhi in Patna would spot Dr Taru out and about with a stethoscope and apparatus to check blood pressure. Her conversations with the pregnant village women revealed a faulty mindset — “We will come to the hospital when there is a complication.” Thus began her endeavour to convince them otherwise. The community baby shower organised by her the following week had a dual intention.
The women were made aware of the importance of maternal health, and routine checkups. “We had 220 pregnant women in our hospital the next day,” she beams. Here’s where she underscores why health systems must be attuned to changing needs.
Skill training is the core of excellent healthcare

Everyone cannot reach a district hospital. So, Dr Taru emphasises, we need skilled healthcare on the peripheries. She believes the government must mandate and enforce the bond requiring medical graduates to be posted in rural areas for a couple of years. “This should apply to everyone including nurses, doctors, Ayurvedic practitioners, and Homoeopathic doctors.” The project, she says, should be spotlighted as heroic, which will boost the morale among medical students.
Optimal use of funds and ensuring accountability
“Back in Mumbai, I used to think our rural hospitals suffered from lack of funds, and corruption led to further dilution of the available money,” Dr Taru shares. So, she was shocked when she learnt that every year Bihar sends back the majority of the PIP (Project Implementation Plan) — yearly funds sanctioned by the Centre to implement health schemes — funds unutilised.
“In 2017, Motihari had used only 12 percent of the funds sanctioned for it,” she learnt. The fallacy was rooted in an antiquated mindset. “Corruption fear meant health officials were extremely reluctant to sanction money for anything. There was a lack of motivation to maintain records, which led to avoidance of using funds. Third, hospital managers are non-technical people, and in the absence of clear feedback from doctors and nurses, they did not know how to use much of the money obtained from these schemes.”

Strengthen the pillars of the medical system — healthcare workers
As skilled as doctors are, last-mile service isn’t always a possibility. Calling ASHA (Accredited Social Health Activist) and Anganwadi workers the arms of the government healthcare system capable of taking healthcare services to the last person in the villages, Dr Taru emphasises proper training be given to them.

“Doctors, no matter how many we have, will never be available to a child with diarrhoea in a remote village at three in the morning. But community-based, well-trained, dedicated ASHAs and Anganwadi workers will. They are the answers for many villages like Masarhi, which are inaccessible due to their geography and poor transport facilities,” she says.

Unwarranted prescription of antibiotics is doing more harm than good
Dr Taru observed how every patient who visited the OPD (Outpatient Department) in the Motihari District Hospital, was prescribed a similar set of pills. One out of these was always an antibiotic. “This occurred after they had already gotten a shot of a high-grade antibiotic,” she points out. This indiscriminate prescribing of medicines by untrained people is brewing an epidemic, she shares, adding that “prolonged use of painkillers can lead to acidity, stomach ulcers, and even kidney damage”.
With every day came a new challenge. And with it, the resolve to change one mindset for the better. Underscoring the impact they were able to create through the community health centre she started and ran at Masarhi, Dr Taru says, “In our first year, we screened 445 children, identified 198 malnourished children and succeeded in bringing 39 of them to normal health.”
In fact, the Motihari District Hospital was awarded the Kayakalp Award in 2018. The award is given by the Indian Ministry of Health and Family Welfare to recognise health centres that promote cleanliness, hygiene, and infection control.

Today, as she looks back, she recalls often being asked “Log to yahaan se Mumbai jaana chahte hain, aap yaha kyu aaye? (People leave this place to go to Mumbai. Why did you leave Mumbai to come here?).” Ironically, the same question perplexed her in 2014 at the outset of her journey. But she sees her time spent in Bihar as liminal.
When she embarked on a quest to revise the contours of healthcare in the state, many dissuaded her. It takes generations for change to happen, they said. You’re asking for too much, others added.
“But the way I see it, a small spark is enough to set a fire ablaze,” she smiles.
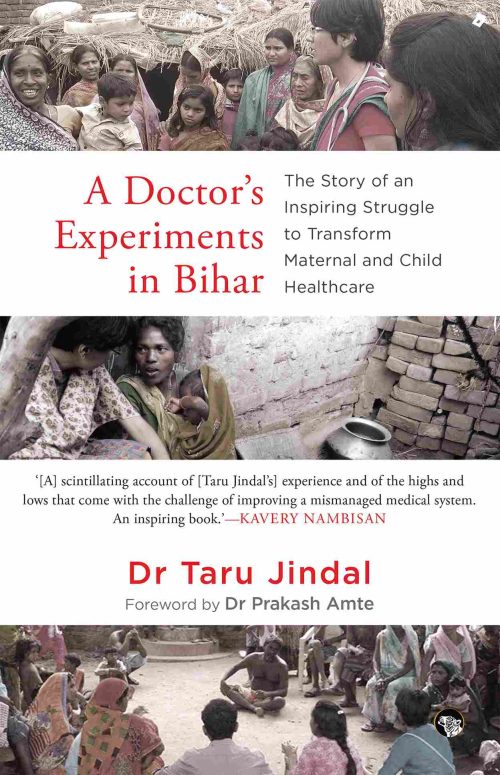
You can read more about Dr Taru’s work in her book ‘A Doctor’s Experiments in Bihar’.
Edited by Khushi Arora; All images courtesy Dr Taru Jindal
No comments:
Post a Comment